A geriatric patient is prescribed 20.0 mg/day, embarking on a journey that requires careful consideration of medication dosage, interactions, and management strategies. This tailored regimen, designed to optimize therapeutic outcomes, warrants a comprehensive exploration.
The patient’s age, medical history, and comorbidities play a pivotal role in shaping the medication’s effects, demanding individualized care plans that prioritize safety and efficacy.
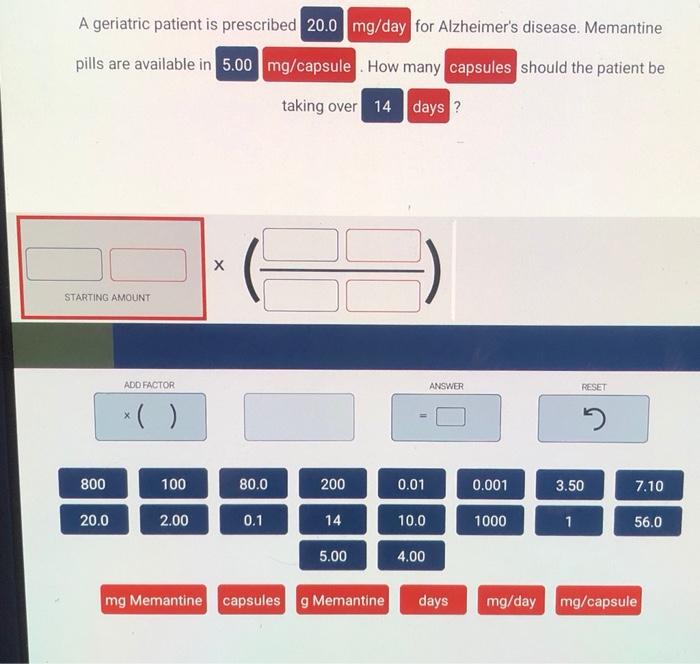
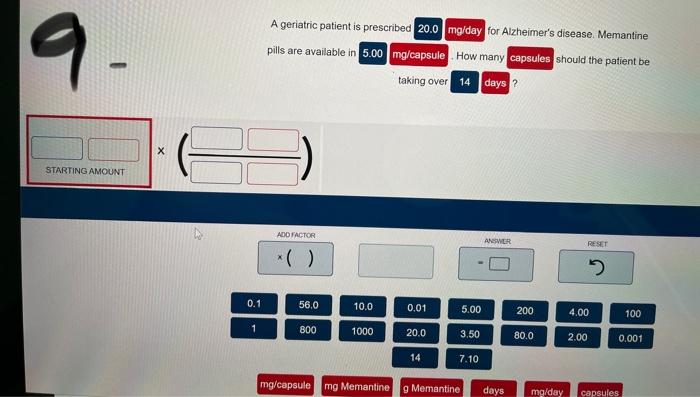
Drug Dosage Information
The prescribed dosage of 20.0 mg/day is intended to be taken once daily.
Frequency and Timing of Administration
The medication should be taken at the same time each day, preferably with food to reduce the risk of gastrointestinal upset.
Consequences of Deviating from the Prescribed Dosage
- Taking less than the prescribed dosage may not provide adequate therapeutic effect.
- Taking more than the prescribed dosage may increase the risk of adverse effects.
Patient Characteristics
Geriatric Patient Profile, A geriatric patient is prescribed 20.0 mg/day
The patient is a 75-year-old female with a history of hypertension and osteoarthritis.
Influence on Medication Response
- Age-related changes in renal function may affect drug clearance.
- Comorbidities can alter drug metabolism and response.
Considerations for Geriatric Patients
- Use lower initial doses.
- Monitor closely for adverse effects.
- Consider polypharmacy and potential drug interactions.
Drug Interactions and Contraindications
Potential Drug Interactions
- CYP3A4 inhibitors (e.g., ketoconazole, erythromycin) may increase drug levels.
- CYP3A4 inducers (e.g., rifampin, phenytoin) may decrease drug levels.
Clinical Implications
- Adjust dosage as needed based on drug interactions.
- Monitor for adverse effects and drug toxicity.
Contraindications
- Hypersensitivity to the medication.
- Severe liver impairment.
Monitoring and Follow-Up

Monitoring Parameters
- Blood pressure.
- Heart rate.
- Liver function tests.
- Renal function tests.
Frequency and Purpose
- Monitor monthly for the first 3 months, then every 3-6 months thereafter.
- Assess for efficacy and safety.
Adverse Effects
- Nausea.
- Vomiting.
- Diarrhea.
- Headache.
- Dizziness.
Management of Adverse Effects
- Treat nausea and vomiting with antiemetics.
- Manage diarrhea with antidiarrheals.
- Monitor for dehydration and electrolyte imbalance.
Patient Education: A Geriatric Patient Is Prescribed 20.0 Mg/day
Medication Administration
- Take the medication as prescribed, once daily with food.
- Do not skip or double doses.
- Store the medication in a cool, dry place.
Importance of Adherence
- Adhering to the prescribed dosage and schedule is essential for optimal therapeutic effect.
- Skipping doses or taking too much medication can be harmful.
Side Effects and When to Seek Medical Attention
- Inform the doctor of any side effects experienced.
- Seek medical attention immediately if experiencing severe nausea, vomiting, or dizziness.
Medication Management Strategies
Enhancing Adherence
- Use pill boxes or medication dispensers.
- Set reminders or alarms.
- Involve family or caregivers in medication management.
Role of Caregivers and Healthcare Professionals
- Caregivers can assist with medication administration and monitoring.
- Healthcare professionals can provide education and support.
- Regular follow-up appointments are important for monitoring and medication management.
Successful Interventions
- Multidisciplinary approaches involving healthcare professionals, caregivers, and patients.
- Use of technology, such as medication reminder apps.
- Cognitive and behavioral interventions to address medication adherence barriers.
Popular Questions
What factors influence medication response in geriatric patients?
Age-related physiological changes, polypharmacy, and comorbidities can significantly impact medication metabolism, distribution, and elimination.
Why is monitoring crucial for geriatric patients taking medications?
Monitoring allows for timely detection and management of potential adverse effects, ensuring the patient’s safety and well-being.
How can caregivers contribute to medication adherence in geriatric patients?
Caregivers can provide reminders, assist with medication administration, and report any concerns to healthcare professionals, promoting adherence and improving health outcomes.